If you’re reading an article titled “How to Sleep”, chances are that you’re stuck in a struggle with sleep and are looking for answers. (If you’re not, well, welcome anyway, and sorry for the confusion… and also, what are you doing here?) I’ve written this guide to help you understand how sleep works and how to apply behavioral sleep medicine principles to improve your sleep. So, basically, how to sleep.
As a behavioral sleep therapist, I make my living by helping people overcome their chronic insomnia problem, utilizing an effective therapeutic intervention called Cognitive Behavioral Therapy for Insomnia. However, I don’t think that just because someone has developed insomnia they automatically need to work with a sleep therapist in order to be able to get their sleep back on track. Also, I don’t think there is just one single, exclusive path towards healthy sleep. That is because our bodies are hardwired to regulate sleep effectively, as sleep is a biological necessity. Our brains are programmed to initiate and maintain sleep at consistent intervals, so this is the default state of things. Therefore I consider insomnia to be not a hardware problem, but a miscalibration of sorts. And overcoming insomnia is simply a process of recalibrating the sleep systems, whether through engaging in behavioral sleep therapy, through self-help resources such as books, workbooks, or apps, or through other ways of tapping into the body’s intrinsic healing mechanisms.
Ingredients for Sleep
In order to recalibrate the sleep systems, I need to first take you through a little bit of sleep science and introduce you to the wonderful biological systems responsible for regulating sleep. I like to think of these as the three key ingredients necessary for sleep to occur. Without these three ingredients being present, you can try all the meditation, aromatherapy, sleepytime tea, weighted blankets, or other life hacks you want—sleep ain’t happening.
The three ingredients necessary for sleep are:
- Sleep Drive: You need to feel sleepy in order to fall asleep. Not just tired (you can be tired and not sleepy), but sleepy like yawning and heavy eyelids. The sleep drive system is your body’s internal sleepiness pressure that builds up throughout the day and dissipates when you sleep. If you have been awake for a long time, you will feel sleepy because your sleep drive accumulates. If your sleep drive is low, you will not be able to sleep.
- Circadian Rhythm: Your circadian rhythm, aka your internal clock, needs to tell you that it’s an appropriate time to sleep. Your clock is maintained and reinforced by behavioral and environmental cues, the most significant being light exposure from the sun cycle. If you travel halfway around the world and induce a bad case of jet lag, your circadian rhythm will be sending alerting signals while it’s nighttime around you, and you will not be able to sleep.
- Relaxation Response: You need to be in a state of relaxation in order to fall asleep. At first this sounds a bit too obvious to be listed as an ingredient, but it is actually quite important. The relaxation response acts as a counterbalance to our body’s stress response, and the stress response has the ability to override sleep/sleepiness. If your body is in a state of threat and the stress response is engaged, you will not be able to sleep.
Now that I’ve briefly introduced the three ingredients for sleep, let me explain each of these systems in a little more detail and describe how we would go about targeting each system in a therapeutic or sleep training context.
The Homeostatic Sleep Drive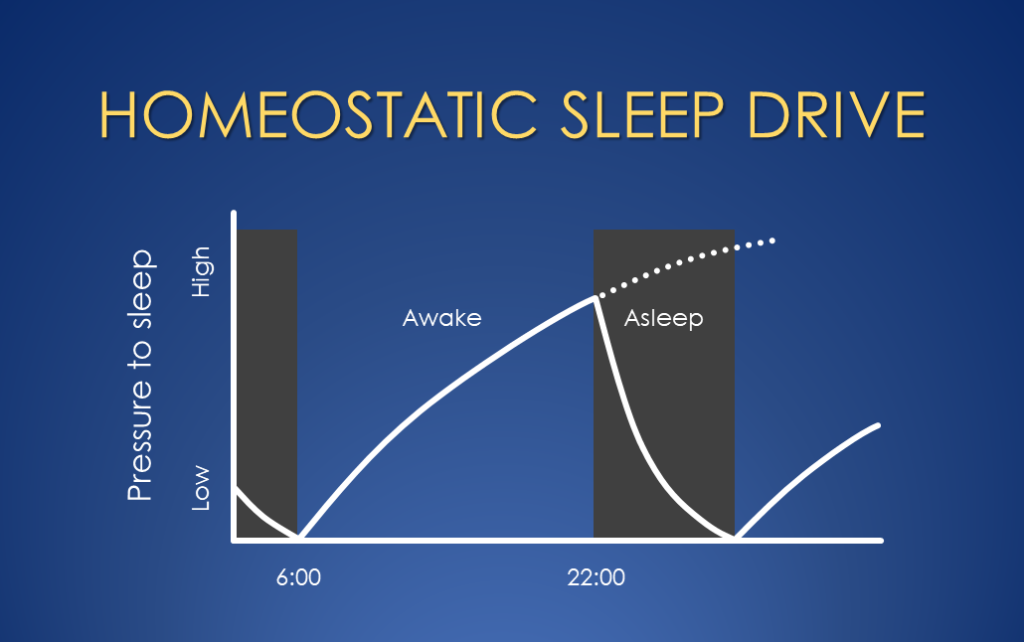
The homeostatic sleep drive is essentially the body’s internal sleepiness pressure that builds up, proportionate to time spent being awake. It is often compared with hunger because those happen to both be primary biological drives that are built in to ensure we adequately attend to the biological necessities of eating and sleeping. After you have sufficiently eaten/slept, your hunger/sleepiness becomes low, and then it gradually builds up over many hours until you feel very hungry/sleepy if you’ve gone too long without food/sleep.
Fascinatingly, there is a neuro-modulator molecule in the brain known as adenosine that is at the heart of the sleep drive system. When you are awake, adenosine molecules increase in concentration in the brain (as a byproduct of brain cells expending energy), and when you are asleep these molecules get used up and decrease in concentration. When the concentration is high it causes decreased metabolic activity in the brain and the physiological changes associated with sleepiness, such as decreased alertness, heavy eyelids, and yawning. Get this: caffeine happens to be a molecule whose structure is just similar enough to adenosine that it can block the neuro-receptors that are responsible for detecting adenosine—effectively “masking” the true sleep drive level and reversing (temporarily) the sleepiness-related physiological changes!
Like I mentioned earlier, you can be tired but not sleepy. These two are often correlated, and in general usage these words are usually interchanged, but they are not the same thing. For people who have developed a chronic problem with insomnia, sleep researchers have observed that they tend to lose the ability to meaningfully distinguish between the two. For years they have felt constantly tired and exhausted from the insomnia struggle, yet when they’re in bed trying to sleep their brains are wide awake and they’re left with no other option but to just try harder to sleep. Sleep research shows that compensatory behaviors such as extending the sleep window (which makes logical sense: it takes me a while to fall asleep, and I’m not getting enough sleep, so I’ll just go to bed earlier) only serve to reinforce and exacerbate this effect. Dependence on sleeping pills also relates to this effect, as insomnia sufferers have conditioned themselves to fall asleep in the presence of the drowsiness caused by the external agent, rather than the internal sleep drive that is dutifully building up in the background.
In behavioral sleep therapy, we target this sleep drive system by seeking to recondition the brain to associate bedtime with a high level of sleep drive. Instead of going to bed tired (but not sleepy) and struggling with frustration and time and effort to fall asleep, we want the brain to get used to the feeling of high sleepiness preceding getting into bed. This does not guarantee that you will fall asleep quickly or have less awakenings immediately, but over time this increased sleep drive pressure does reliably translate to falling asleep faster and staying asleep better.
How does one increase sleep drive before bedtime, you may ask? This brings us to one of the core behavioral sleep techniques, one which I call “compressing the sleep window” (but in sleep textbooks goes by the name “sleep restriction therapy”). This technique is simply to reduce your time in bed by anchoring the wake up time and pushing your bedtime later. How much later? Later enough that you start to notice increased sleep drive pressure accumulating, but not too much that you’re a zombie during the day, sleep past your alarms, and keep dozing off before your bedtime. In therapy we utilize sleep logs to calculate a more data-informed bedtime and wake-up time, but you can fairly easily guesstimate this on your own.
Another way to increase nighttime sleep drive is by eliminating naps, if they’re a common occurrence. There is nothing inherently wrong with taking naps (naps are sleep, and sleep is recovery, which is positively good), but while we’re recalibrating your sleep systems, our primary objective here is accumulating nighttime sleep drive—which naps will sabotage. In this context, taking a nap is like eating a snack before dinner because you’re so hungry. By the time dinner is served, that hunger is significantly lower and you’ve lost your big appetite.
The Circadian Rhythm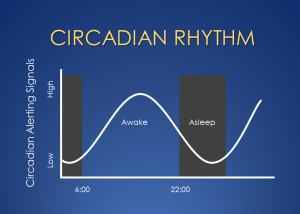
The circadian rhythm is your body’s internal 24-hour clock, and it’s headquartered in a small region of your brain’s hypothalamus called the suprachiasmatic nucleus (SCN), but its reach is felt in every major organ system. The circadian system is not exclusively a sleep system, but it regulates the timing of many other biological rhythms, such as body temperature, metabolism, digestion, hormone release, and immune regulation. (Technically this term should be pluralized to “circadian rhythms” and rigorous scientists and academics make sure to get it right, but I find it easier to talk about it as a singular system, so I’ll claim creative license as a clinician.) As it relates to the sleep/wake cycle, the circadian rhythm has a “day mode”, during which it sends alerting signals and generally tries to keep you awake and active, and a “night mode” during which metabolism and activity decrease, and sleepiness and relaxation prevail. The darkness-signaling hormone melatonin is released when the light levels signal that the sun has gone down, and this ushers in the circadian “night mode”.
The circadian rhythm is programmed to keep us synchronized to the day-and-night cycle, essentially keeping us anchored to our home time zone. Fascinatingly, this internal clock will continue the daily 24-hour cycles of sleep-wake and other circadian activity even in the absence of sunlight and other time cues—which early sleep researchers studied by locking themselves in a dark basement for weeks—but over time the internal clock will drift out of sync with the external day-and-night cycle because it turns out that the clock is a roughly, not precisely, 24-hour clock. It relies regularly on the cues provided by the sun cycle to keep it in sync. This is precisely both why we experience jet lag (friction from the mismatch between the body’s internal clock and the new environmental cues) and how jet lag automatically resolves itself in a matter of days (the internal clock gets pulled to match the new sun cycle).
If you’ve noticed, I’ve talked about the sun a lot so far in my explanation of the circadian rhythm. This is because light exposure is the primary and most important external cue that our circadian rhythm relies on. There are other cues that can influence the circadian rhythm—such as meal times, exercise, and temperature—but these are much, much weaker compared to the outsized effect that light exposure has on the circadian rhythm. Scientists have worked out the exact effect of light based on the timing in relation to one’s circadian cycle, and they describe it as a phase response curve. My simplified explanation is that there are two “light-sensitive periods” over the 24-hour day: the first few hours after waking up and the last few hours before falling asleep. During these periods, the circadian rhythm is especially sensitive to light information, which it uses to make adjustments to the internal clock as necessary. Essentially, it’s looking for bright light in the morning right after waking up (to validate that the sun has come up when the circadian rhythm expected it to), and lower light levels in the evening hours leading up to bed (to validate that the sun has gone down as expected).
In sleep therapy, there are two primary ways we target the circadian rhythm. The first is by keeping a consistent sleep/wake schedule. Waking up at the same time every morning and going to bed at the same time every night ensures that you’re setting the timer for the start of the circadian day and the start of the circadian night consistently. And this means that you’re strengthening the circadian signals that coordinate the transitions between the circadian day and night modes. In other words, if our goal is to get clear and consistent output signals regarding the timing of the circadian day and night modes, we need to reinforce it with consistent input signals. (Being roughly or approximately consistent with your sleep/wake times is good enough, and in fact, being overly rigid may prove to be counterproductive if this ends up increasing stress and effort around sleep.)
The second way we target the circadian rhythm is by modulating light exposure during those two light-sensitive periods: first few hours after waking up and last few hours before bed. Remember that light exposure is the single most important external cue that the circadian rhythm relies on. During the two transition periods marking the start of the circadian day and the start of the circadian night, we have the ability to strengthen the circadian timing signals by reinforcing the light cues that the system is looking for. In the mornings, you should open the blinds, turn on bright lights, and get sunlight if possible, all within the first hour or so of waking up. In the last few hours before bed, you should dim your indoor lighting level about halfway, turning off bright white overhead lights and instead using warmer/softer light sources, and dim the brightness on your backlit devices (also use blue-blocking settings if you can). Finally, I recommend stopping the use of backlit screens 30 minutes before bedtime (which I have found to be more reasonable and just as effective as having a 1-hour ban). Remember you are trying to mimic the natural conditions our brains are programmed to detect before industrialization and artificial lighting got in the way. The bright light in mornings and dim light in evenings are two sides of the same coin and are both critical in this process—what scientists call circadian entrainment and what I call recalibrating the circadian rhythm.
The Relaxation Respons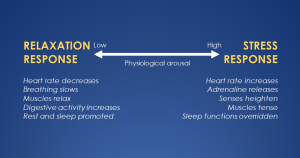 e
e
The relaxation response is known formally as the parasympathetic branch of the autonomic nervous system (you can see why I stick with calling it the relaxation response), and it is activated during periods of rest, recovery, and digestion. Its counterpart is the stress response, known formally as the sympathetic branch. The stress response gets activated when your brain perceives danger or threat, and it mobilizes the body’s physiological resources to prepare for immediate action—heart rate increasing, blood vessels constricting, and stress hormones pumping. These two branches provide a counterbalance to each other, and in any given moment you can physiologically be in any state along this continuum, between utter relaxation and extreme stress (“fight or flight”), depending on what your brain perceives is needed in that moment. Stress typically gets a bad rap, but you’ve got to keep in mind that the stress response is critically important to helping us respond quickly to challenges, from facing physical threats to dealing with high-pressure situations or solving complex problems. We literally need it to survive. Thus, it’s the push-and-pull between the stress response and the relaxation response that allows our bodies to navigate the demands of life and maintain a balance between action and recovery.
Where does this fit in with sleep? Well, as you might have guessed, sleep falls under the domain of the relaxation response. Rest, recovery, and sleep are functions of the parasympathetic nervous system and need this system to be engaged. In other words, you need to be in a physiological state of relaxation in order for sleep to occur.
What’s more, the stress response has the ability to essentially veto the other two sleep systems and to override sleep and sleepiness. From a survival perspective, this makes perfect sense: you want your brain to prioritize safety over sleep when you are faced with a threat. Let’s do a thought experiment and imagine that you are camping with your family and are just starting to drift off peacefully to sleep with the exhaustion of a long day’s hike, when suddenly you hear some scratching outside your tent and the unmistakable low growl of a wild animal. Instantaneously, as the hairs on the back of your neck stand up, you will feel the stress hormones coursing through your body, all of your senses will become extremely heightened, and any shred of sleepiness will have vanished into thin air. Where did it go? The other two ingredients for sleep are surely intact—the sleep drive level is still high, the circadian rhythm is still in night mode—as these things cannot suddenly change or go away. It’s the third ingredient that has suddenly changed; the relaxation response was interrupted by the stress response, which overrode sleepiness to prioritize survival.
Now, I realize that you’re not going to be facing such an extreme stress response most nights. The point was just to illustrate that the stress response has the ability to override sleep. However, my guess is that if you’re experiencing persistent trouble sleeping, you’ll be able to identify with some or many of these factors that can elevate the stress response: anxiety about the next day, worry about not being able to sleep, strong emotions such as anger or fear, ruminating negative thoughts, relational conflict, physical pain/discomfort, and more. While these may not be at a “fight or flight” level like the camping example, these kinds of stressors still do override sleepiness (albeit to a lesser extent) and increase the struggle to fall asleep. The stress response increases arousal in the brain and tells it that sleep is not a good idea right now because there is a problem that first needs to be dealt with.
Therefore, in sleep therapy, our objective is to consistently reinforce bedtime with the relaxation response. This means consistently engaging the relaxation response prior to getting into bed, both in order to decrease stress response activity and also to strengthen the brain’s connection between bedtime and relaxation. We want to help the brain make the relaxation response the default response associated with bedtime. My advice is to set aside approximately the last 30 minutes before bed to be a “wind-down” period, during which you (in addition to not using backlit screens) engage in physical relaxation and mental relaxation. I’m not offering a specific method or set of instructions—just do something physically relaxing and something mentally relaxing that works for you.
Some ideas for physical relaxation: gentle stretching, warm shower/bath, self-massage, foam roller, relaxing yoga, breathing exercise, progressive muscle relaxation, body scan, etc. Some ideas for mental relaxation: reading a book, listening to audiobook or podcast, puzzles (crossword, sudoku, jigsaw), herbal tea with a loved one, mindfulness meditation, guided imagery exercise, gratitude journal, nature sounds, etc. Don’t get hung up on trying to make it perfect. It’s not about picking exactly the right things—there are multiple ways to get to a relaxed state, and everyone is different—but it’s about consistently setting aside this time to relax and teach your brain this new pattern related to bedtime.
One common pitfall that I want to caution you about is using relaxation as a method to try to control sleep. Intention is key here. You must learn to engage in relaxation with the simple objective of conditioning your brain to see bedtime as a relaxing time, and not with the objective of making sleep happen more quickly. If you’ve been stuck in an insomnia struggle for a long time, your brain likely sees sleep as a nightly battle it must fight, and it will tend to try to wield even relaxation as a weapon to deploy in the battle with sleep. The problem is that: 1) we cannot directly control sleep no matter how hard we try, and 2) this only serves to increase hyperarousal and activate the stress response. When you use relaxation strategies with the goal of falling asleep, your brain operates with the implicit message that there is a problem here (not sleeping) that you are trying to fix. The stress response says: “There’s a problem here? Let me help you with that…” Instead, relaxation is an invitation to slowly let go of the struggle that has defined your relationship with sleep, to relieve the stress response of its role when it comes to trying to sleep. Engage in relaxation-promoting activities with the simple aim of teaching your brain that relaxation consistently precedes bedtime.
Consistent Conditions, Low Effort
This dovetails perfectly to the larger point of all of these recalibration efforts. You are simply trying to teach your brain through repeated reinforcement that the ingredients for sleep are naturally present by the time you get into bed. That’s it! By increasing the sleep drive associated with bedtime, by strengthening the circadian rhythm through consistent sleep/wake timing and with light exposure modulation, and by engaging in relaxation before bed, you consistently create the conditions necessary for sleep, and your brain begins to learn that sleep is a phenomenon that happens naturally when the conditions are right. Your brain starts to trust the sleep systems to do their job, and it starts to let go of the effort and struggle surrounding sleep. This obviously does not happen all at once, but it does happen a lot more quickly than you would expect given how long the typical person with insomnia has been struggling with it.
And the training is definitely meant to be short-term, not indefinite. For example, with compressing the sleep window, we push the bedtime later in order to accumulate more sleep drive in the short term, but typically within a few weeks we start to expand the sleep window back out at a gradual pace. And the rest of the behavioral changes we introduce to target the sleep systems can be thought of as implementing structure to help the sleep pattern to stabilize and the sleep effort to decrease, but over time the structure should gradually loosen and fade away. The end goal isn’t to make you follow an extensive list of rules forever in order to sleep well, it’s to recalibrate your sleep systems and tap into their ability to regulate sleep in a robust and resilient way.
My aim in this article was to teach you how to sleep by introducing you to the three key ingredients for sleep and the science of how sleep works. By targeting these very systems we can effectively recalibrate them and regain a stable sleep pattern, essentially getting back to the way that sleep is supposed to function. Of course, this process is much more nuanced and personalized in a therapeutic context, because each person’s struggle with sleep has its own history and context. However, because the biology of sleep is a consistent factor across individuals, learning about the sleep systems and implementing steps to recalibrate them remains an extremely powerful part of behavioral sleep therapy.
Whether you are a good sleeper or struggle with sleep, I hope you gained some valuable knowledge about the inner workings of sleep, confidence in your body’s innate ability to regulate sleep, and behavioral tools to help you restore a healthy sleep pattern.